CBD Oil
Earn 135.00 points on this purchase
CBD Oil
Our CBD oil, made with the best Oregon-grown hemp, is a supplement for rejuvenating your body and mind. Each batch is made from a refined broad-spectrum extract. Feel free to choose between our fan-favorite mint, citrus, natural, strawberry, and cookies & cream flavors.

Closer Look at CBD Oil
CBD-infused oil is an extract of hemp, mostly derived from the stem, leaves, and flowers. Hemp growers harvest it after about 120 days, which is around the end of the flowering period. The plants are cut near the root and left out to dry. Once dry, the stems are soaked so that the fibers in them can soften and go through decortication, which is the process of separating the fibers from the stem.
After decortication, CBD is extracted using a variety of methods. One of the safest methods is CO2 extraction, but they can also use oil extraction or ethanol extraction. Each method has its merits and drawbacks. After the extraction, the CBD contains many undesirable elements such as waxes and lipids. The extract must undergo distillation to remove these unnecessary elements.
After distillation, the extract is diluted with a base or carrier oil, such as coconut oil, to facilitate easier absorption by the body. Hence the name CBD oil. You can buy the oil in many different flavors, as the natural oil's taste tends to be intense. The taste is also the reason some people add it to edibles.
Description
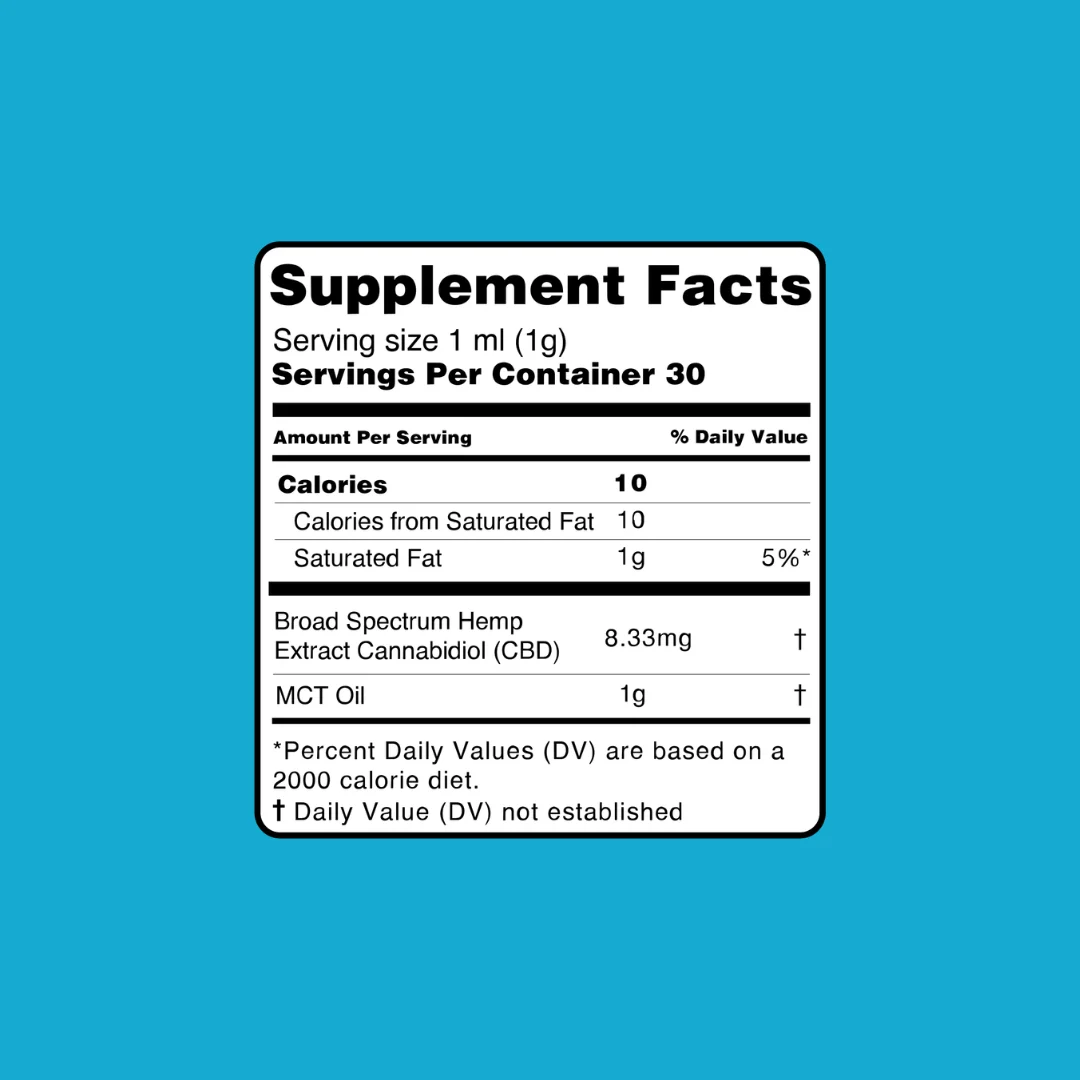
Our broad-spectrum oil is available in four strengths (250mg, 600mg, 1,000mg, and 2,500mg) and five great flavors (mint, citrus, strawberry, cookies & cream, and natural). It’s always made to order. That means when you buy CBD oil from us, it will always arrive fresh at your door.
Ingredients
Hemp Oil, MCT Oil, Natural Flavor, Terpenes

Suggestions
While the dropper is inside the bottle, squeeze the rubber end and release it to let it fill back up as far as it will go. This should fill up to around half of the dropper, providing a full 1ml dose of the oil.
For the best results, place one full dose under the tongue and wait 60-90 seconds before swallowing. Alternatively, it can also be mixed with food and drink. Take once or twice daily.
It is always recommended to talk to your doctor first before you start using CBD, in much the same way you would with any supplement to your diet. Their guidance should help with determining the best amount for you.
Return Policy
A full refund is available for all UNOPENED products. All you have to do is ship the products back within 30 days of your purchase. A shipping label is provided for returns upon request.

Storage
It is recommended that you store your CBD oil bottle in a cool, dark and dry place such as a pantry or cupboard. Exposure to excessive levels of heat, light, and moisture may cause evaporation and subsequent degradation of the oil, reducing its shelf life.
The same goes for any other CBD products that you might have.
If you choose to keep the bottle in a refrigerator, it may thicken and require heating before use. In that case, simply run warm water over the bottle for a moment. It is not advised to keep this product in the freezer, though.
What Makes Our CBD Oil Different?
Full Spectrum Hemp Extract
We use full-spectrum hemp extract that includes cannabinoids, terpenes, and trace amounts of THC (less than 0.3%) to promote the entourage effect—a synergistic benefit that enhances the oil’s impact.
Organic MCT Oil for Better Absorption
Our carrier oil of choice is organic MCT oil. It enhances bioavailability, ensuring that cannabidiol is efficiently absorbed when taken sublingually or mixed with food.
Tested for Purity and Potency
Every batch of our Cannabidiol oil is third-party lab tested for cannabinoid content, pesticides, heavy metals, and other contaminants. We aim to provide the highest quality product without compromise.
Benefits of CBD Infused Oil You Can Count On
Natural Pain Relief
Scientific studies have shown that cannabinoids can support chronic pain relief by interacting with the body’s endocannabinoid system. Whether it's joint discomfort or post-workout soreness, CBD-infused oil may provide a natural alternative.
Promotes a Calmer Mind
The oil is widely used to help with anxiety, and early research suggests it may influence serotonin receptors that regulate mood. It’s a gentle, non-psychoactive way to restore calm.
Supports Overall Health and Immunity
Rich in fatty acids and derived from USA-grown hemp, our Spectrum Cannabinoid-rich oil may aid in maintaining a healthy immune response and reducing inflammation associated with common health concerns.
Effective Usage
The usage of CBD varies from person to person. People experience different side effects from it and use it for various purposes, so there is no set dosage that is recommended. What users are commonly advised to do is to use the trial-and-error method. This involves two main steps:
Start by taking the lowest dose you can and wait to see the effects. Increase the amount slowly until you feel that it is meeting your needs.
Start by taking the magical Cannabinoid-rich oil in the evening. You don't know what type of effect it will have on you, so you shouldn't risk using it during the day when it may cause some negative consequences.
Many people use it directly, while others use it to make edibles such as gummies, pastries, and even capsules. The two rules above apply no matter how you are ingesting it.
Concentration in the CBD oil.
Why Choose Penguin Wellness CBD Oil?
Full-spectrum hemp extract with a rich cannabinoid profile
Blended with organic MCT oil for superior absorption
Third-party lab tested for potency and purity
Clean, high-quality formulas free from harmful additives
Trusted by thousands and recommended in top CBD reviews
Explore more ways to incorporate CBD into your routine with our CBD for better sleep solutions.
CBD Oil FAQ
Ultimate CBD Oil Buying Guide

Third-Party Lab Report
Our CBD oil for sale has been thoroughly tested by an ISO 17025 accredited, third-party independent lab. They ensure that our products contain zero pesticides, heavy metals or harmful contaminants. If you wish to check the results yourself, click here.